Ditch the paperwork to keep pace with patient care.
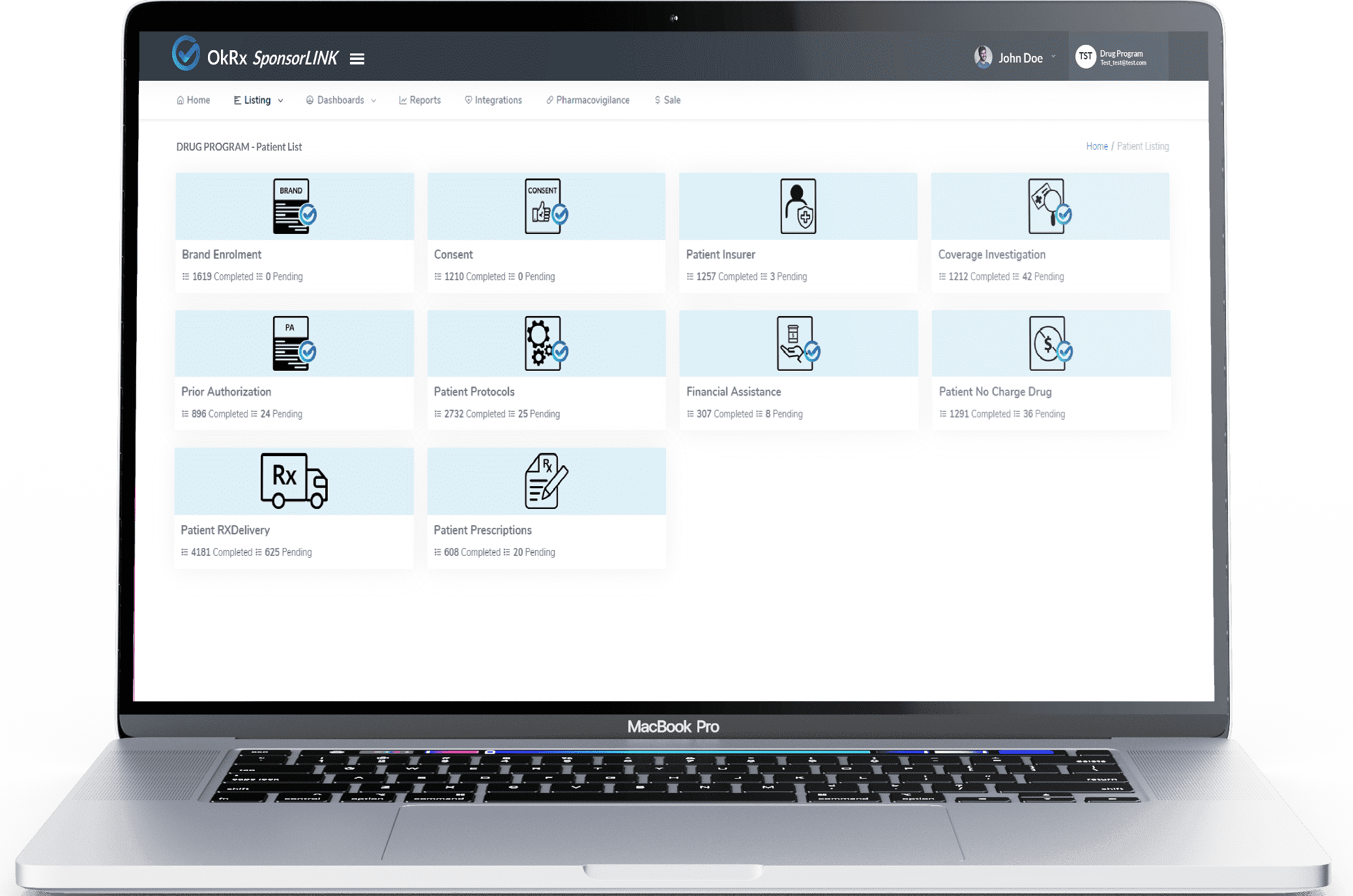
Instead of drowning in Prior Authorization faxes and phone calls, OkRx can facilitate clinical and financial information needed to assess Prior Authorizations securely and electronically. Our electronic process eliminates manual workflows while reducing the cost per case for insurers, while ensuring plan members and their families receive responses they need faster.